Office chair
From Wikipedia, the free encyclopedia
| This article needs additional citations for verification. Please help improve this article by adding reliable references. Unsourced material may be challenged and removed. (February 2009) |
| This article's introduction section may not adequately summarize its contents. To comply with Wikipedia's lead section guidelines, please consider expanding the lead to provide an accessible overview of the article's key points. (September 2009) |
Contents[hide] |
History
One the earliest known innovators to have created the modern office chair was naturalist Charles Darwin, who put wheels on the chair in his study so he could get to his specimens more quickly.[1]With the advent of rail transport in the mid-19th century, businesses began to expand beyond the traditional model of a family business with little emphasis on administration. Additional administrative staff was required to keep up with orders, bookkeeping, and correspondence as businesses expanded their service areas. While office work was expanding, an awareness of office environments, technology, and equipment became part of the cultural focus on increasing productivity. This awareness gave rise to chairs designed specifically for these new administrative employees: office chairs. This caught the attention of Otto von Bismarck, who is credited with popularizing the office chair by distributing them throughout parliament during his time in office.
The office chair was strategically designed to increase the productivity of clerical employees by making it possible for them to remain sitting at their desks for long periods of time. A swiveling chair with casters allowed employees to remain sitting and yet reach a number of locations within their work area, eliminating the time and energy expended in standing. The wooden saddle seat was designed to fit and support the body of a sitting employee, and the slatted back and armrests provided additional support to increase the employee’s comfort. Like modern chairs, many of these models were somewhat adjustable to provide the maximum comfort and thus the maximum working time.
Ergonomics
In the 1970s, ergonomics became an important design consideration. Today, office chairs often have adjustable seats, armrests, backs, back supports, and heights to prevent repetitive stress injury and back pain associated with sitting for long periods. Ergonomic chairs fit an individual's needs and provide support where the individual needs it. New concepts of office chairs include a seat oscillating forwards and sideways and an oscillating seat back to allow the body to move as much as possible during sitting. [2]Task chair
A task chair is a type of office chair that is commonly used in conjunction with an office desk. These chairs have multiple adjustments to be able to be used by many different users.[Low back pain
From Wikipedia, the free encyclopedia
| This article contains instructions, advice, or how-to content. The purpose of Wikipedia is to present facts, not to train. Please help improve this article either by rewriting the how-to content or by moving it to Wikiversity or Wikibooks. (July 2010) |
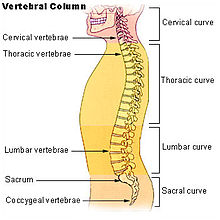
The five vertebrae in the lumbar region of the back are the largest and strongest in the spinal column. | |
| ICD-10 | M54.4-M54.5 |
|---|---|
| ICD-9 | 724.2 |
| MedlinePlus | 003108 |
| eMedicine | pmr/73 |
| MeSH | D017116 |
Contents[hide] |
[edit] Classification
One method of classifying lower back pain is by the duration of symptoms: acute (less than 4 weeks), sub acute (4–12 weeks), chronic (more than 12 weeks).[edit] Cause
Most cases of lower back pain are due to benign musculoskeletal problems and are referred to as non specific low back pain. They are generally believed to be due to a sprain or strain in the muscles of the back and the soft tissues,[2] especially if the pain arose suddenly during physical load to the back, and the pain is lateral to the spine. The rate of serious causes is less than 1%.[3] The full differential diagnosis includes many other less common conditions.- Mechanical:
- Apophyseal osteoarthritis
- Diffuse idiopathic skeletal hyperostosis
- Degenerative discs
- Scheuermann's kyphosis
- Spinal disc herniation ("slipped disc")
- Spinal stenosis
- Spondylolisthesis and other congenital abnormalities
- Fractures
- Leg length difference
- Restricted hip motion
- Misaligned pelvis - pelvic obliquity, anteversion or retroversion
- Abnormal Foot Pronation
- Inflammatory:
- Seronegative spondylarthritides (e.g. ankylosing spondylitis)
- Rheumatoid arthritis
- Infection - epidural abscess or osteomyelitis
- Neoplastic:
- Bone tumors (primary or metastatic)
- Intradural spinal tumors
- Metabolic:
- Osteoporotic fractures
- Osteomalacia
- Ochronosis
- Chondrocalcinosis
- Referred pain:
- Pelvic/abdominal disease
- Prostate Cancer
- Posture
[edit] Pathophysiology
The lumbar region (or lower back region) is made up of five vertebrae (L1-L5). In between these vertebrae lie fibrocartilage discs (intervertebral discs), which act as cushions, preventing the vertebrae from rubbing together while at the same time protecting the spinal cord. Nerves stem from the spinal cord through foramina within the vertebrae, providing muscles with sensations and motor associated messages. Stability of the spine is provided through ligaments and muscles of the back, lower back and abdomen. Small joints which prevent, as well as direct, motion of the spine are called facet joints (zygapophysial joints).[4]Causes of lower back pain are varied. Most cases are believed to be due to a sprain or strain in the muscles and soft tissues of the back.[2] Overactivity of the muscles of the back can lead to an injured or torn ligament in the back which in turn leads to pain. An injury can also occur to one of the intervertebral discs (disc tear, disc herniation). As the body ages, the spine does as well. Due to aging, discs begin to diminish and shrink in size, resulting in vertebrae and facet joints rubbing against one another. Ligament and joint functionality also diminishes as one ages, leading to spondylolisthesis, which causes the vertebrae to move much more than they should. Pain is also generated through spinal stenosis, sciatica and scoliosis. At the lowest end of the spine, some patients may have tailbone pain (also called coccyx pain or coccydynia). Others may have pain from their sacroiliac joint, where the spinal column attaches to the pelvis, called sacroiliac joint dysfunction. Physical causes may include osteoarthritis, rheumatoid arthritis, degeneration of the discs between the vertebrae or a spinal disc herniation, a vertebral fracture (such as from osteoporosis), or rarely, an infection or tumor.
In the vast majority of cases no noteworthy or serious cause is ever identified. Usually the pain resolves on its own after a few weeks. Intensive testing for a physical cause without waiting for the pain to recede is not prudent because any problems identified may be irrelevant and misleading.[5]
[edit] Diagnostic approach
Acute back pain is defined as pain less than 6 weeks while chronic back pain is defined as pain that has been present for over three months. The intermediate time period is known as sub acute back pain.[6] Determination of the underlying cause is usually made through a combination of a medical history, physical examination, and, when necessary, diagnostic testing, such as an x-ray, CT scan, or MRI.[edit] Imaging
From 1994 to 2006, MRI scans of the lumbar region increased by 307%.[7] Imaging rates and surgery rates are directly related. Where imaging rates are highest in the country, surgery rates are the highest.[8] The American College of Physicians as well as the American Pain Society both highly advise against consistent imaging in patients who deal with nonspecific low back pain.[9] However, the use of MRI and CT scans is recommended when a patient deals with consistent leg and back pain.[9] There is no relation between MRI/CT scans and positive patient outcomes.[10]X-ray
X-rays are useful in determining deformities in one's bones. They can provide one with the most obvious causes of low back pain due to bone fractures or changes in bone due to aging.
Bone density test
Osteoporosis does not cause low back pain; however, bone fractures may occur due to osteoporosis, resulting in low back pain.
X-rays and CT scans are not required in lower back pain except in the cases where "red flags" (listed below) are present.[11] If the pain is of a long duration X-rays may increase patient satisfaction.[12]
[edit] Red flags
- Recent significant trauma
- Milder trauma if age is greater than 50 years
- Unexplained weight loss
- Unexplained fever
- Previous or current cancer
- Intravenous drug use
- Osteoporosis
- Chronic corticosteroid use
- Age greater than 70 years
- Focal neurological deficit
- Duration greater than 6 weeks[13]
[edit] Prevention
Low back pain is common and there are several methods of prevention. Although exercise show conflicting results in treatment of acute episodes, it is effective in preventing recurrences.[14] Proper lifting technique may also be important.[15]A number of studies were conducted about the relationship between the spine and nicotine. Cigarette smoking is a factor that inversely affects the success and proper healing of spinal fusion surgery. In patients who underwent cervical fusion, a smokers rate of nonunion was much greater than a nonsmoker.[16] Smoke and nicotine cause the spine to age faster than normal. Smoking also reduces blood flow to the lower spine and causes the spinal discs to degenerate.[17]
[edit] Management
[edit] Conservative
For the vast majority of people, low back pain can be treated conservatively. A number of recommendations which may help alleviate symptoms include:[18] applying heat or cold,[19][20] physical therapy,[21] and continued activity within the limits of the pain with bed rest being discouraged.[22] Firm mattresses are less likely to lead to improvement when compared with a medium-firm mattress.[23][edit] Acute back pain
- Medications
- Activity
- Spinal manipulation
[edit] Chronic back pain
Low back pain is more likely to be persistent among people who previously required time off from work because of low back pain, those who expect passive treatments to help, those who believe that back pain is harmful or disabling or fear that any movement whatever will increase their pain, and people who have depression or anxiety.[5] A systematic review (2010) published as part of the Rational Clinical Examination Series in the Journal of the American Medical Association reviews the factors that predict disability from back pain.[39] The data quantified that patients with back pain who have poor coping behaviors or who fear activity are about 2.5 times as likely to have poor outcomes at 1 year.The following measures have been found to be effective for chronic non-specific back pain :
- Exercise appears to be slightly effective for chronic low back pain.[40] The Schroth method, a specialized physical exercise therapy for scoliosis, kyphosis, spondylolisthesis, and related spinal disorders, has been shown to reduce severity and frequency of back pain in adults with scoliosis.[41]
- Tricyclic antidepressants are recommended in a 2007 guideline by the American College of Physicians and the American Pain Society.[42]
- Acupuncture may help chronic pain[25]; however, a more recent randomized controlled trial suggested insignificant difference between real and sham acupuncture.[43]
- Intensive multidisciplinary treatment programs may help subacute[24] or chronic[25] low back pain.[5]
- Behavioral therapy[25]
- The Alexander Technique was shown in a UK clinical trial to have long term benefits for patients with chronic back pain.[44]
- Back schools have shown some effect in managing chronic back pain.[45]
- Spinal manipulation was shown to have a clinical effect similar to that of other commonly used therapies and was considered safe.[46]
- Clinical research shows that treatment according to McKenzie method is as effective as other commonly used methods[47][48][49][50][51][52][53][54][55]
[edit] Surgery
Surgery may be indicated when conservative treatment is not effective in reducing pain or when the patient develops progressive and functionally limiting neurologic symptoms such as leg weakness, bladder or bowel incontinence, which can be seen with severe central lumbar disc herniation causing cauda equina syndrome or spinal abscess.[citation needed] Spinal fusion has been shown not to improve outcomes in those with simple chronic low back pain.[59]The most common types of low back surgery include microdiscectomy, discectomy, laminectomy, foraminotomy, or spinal fusion. Another less invasive surgical technique consists of an implantation of a spinal cord stimulator and typically is used for symptoms of chronic radiculopathy (sciatica). Lumbar artificial disc replacement is a newer surgical technique for treatment of degenerative disc disease, as are a variety of surgical procedures aimed at preserving motion in the spine. According to studies, benefits of spinal surgery are limited when dealing with degenerative discs.[60]
A medical review in March 2009 found the following: Four randomised clinic trials showed that the benefits of spinal surgery are limited when treating degenerative discs with spinal pain (no sciatica). Between 1990 and 2001 there was a 220% increase in spinal surgery, despite the fact that during that period there were no changes, clarifications, or improvements in the indications for surgery or new evidence of improved effectiveness of spinal surgery. The review also found that higher spinal surgery rates are sometimes associated with worse outcomes and that the best surgical outcomes occurred where surgery rates were lower. It also found that use of surgical implants increased the risk of nerve injury, blood loss, overall complications, operating times and repeat surgery while it only slightly improved solid bone fusion rates. There was no added improvement in pain levels or function.[61]
Spinal fusion
The logic behind spinal fusion is that by fusing two vertebrae together, they will act and function as a solid bone. Since lumbar pain may be caused by excessive motion of the vertebra the goal of spinal fusion surgery is to eliminate that extra motion in between the vertebrae, alleviating pain. If scoliosis or degenerative discs is the problem, the spinal fusion process may be recommended. There are several different ways of performing the spinal fusion procedure; however, none are proven to reduce pain better than the others.[21]
[edit] Some or no benefit
Additional treatments have been more recently reviewed by the Cochrane Collaboration:- Heat application may have a modest benefit. The evidence for cold therapy is limited.[63]
- Correcting leg length difference may help by inserting a heel lift or building up the shoe.[66]
- A 2008 review found antidepressants ineffective in the treatment of chronic back pain[68] even though some previous studies did find them helpful.[25]
- Transcutaneous electrical nerve stimulation (TENS) has not been found to be effective in chronic lower back pain.[69]
[edit] Prognosis
Most patients with acute lower back pain recover completely over a few weeks regardless of treatments.[70][71] With the usual lumbar muscle strain or sprain as the cause, over 90% of patients are completely recovered within one month.[72] Although an episode of lower back pain may settle quickly, recurrence rates are about 50% in the following 12 months. About 2% of the population with low back pain are temporarily or chronically disabled by their form of low back pain. 41% of adults aged between 26 and 44 years reported having back pain in the previous 6 months. Most had occasional episodes of pain that lasted a few days, was mild or moderate in intensity, and did not limit activities. Although a high percentage of individuals have persistent lower back pain, 75% of them self-manage their problem and a few become significantly disabled by low back pain. In the United States, the costs of low back pain range between $38 and $50 billion a year and there are 300,000 operations annually. Along with neck operations, back operations are the 3rd most common form of surgery in the United States.[73][edit] Epidemiology
Over a life time 80% of people have lower back pain,[71] with 26% of American adults reporting pain of at least one day in duration every three months.[74][edit] In pregnancy
50-70% of all pregnant women experience back pain.[75]As one gets farther along in the pregnancy, due to the additional weight of the baby, one’s center of gravity will shift forward causing one’s posture to change. This change in posture leads to increasing lower back pain.[76][77]
The increase in hormones during pregnancy is in preparation for birth. This increase of hormones softens the ligaments in the pelvic area and loosens joints. This change in ligaments and joints may alter the support in which one’s back is normally used to.[78][79]
[edit] See also
[edit] References
- ^ "Lower Back Pain Fact Sheet. nih.gov". http://www.ninds.nih.gov/disorders/backpain/detail_backpain.htm. Retrieved 2008-06-16.
- ^ a b irishhealth.com > Lumbago Retrieved on Dec 25, 2009
- ^ Henschke N, Maher CG, Refshauge KM, et al. (October 2009). "Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain". Arthritis Rheum. 60 (10): 3072–80. doi:10.1002/art.24853. PMID 19790051.
- ^ Floyd, R., & Thompson, Clem. (2008). Manual of structural kinesiology. New York, NY: McGraw-Hill Humanities/Social Sciences/Languages.
- ^ a b c d Atlas SJ (2010). "Nonpharmacological treatment for low back pain". Journal of Musculoskeletal Medicine 27 (1). http://www.musculoskeletalnetwork.com/display/article/1145622/1507555.
- ^ Bogduk M (2003). "Management of chronic low back pain". Medical Journal of Australia 180 (2): 79–83. PMID 14723591. http://www.mja.com.au/public/issues/180_02_190104/bog10461_fm.html.
- ^ Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: time to back off? J Am Board Fam Med 2009; 22: 62–8.
- ^ Lurie JD, Birkmeyer NJ, Weinstein JN. Rates of advanced spinal imaging and spine surgery. Spine 2003; 28: 616–20.
- ^ a b Chou R, Qaseem A, Snow V, Casey D, Cross JT, Shekelle P, Owens DK. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007; 147: 478–91.
- ^ Gilbert F, Grant A, Gillan M, et al. Scottish Back Trial Group. Low back pain: influence of early MR imaging or CT on treatment and outcome—multicenter randomized trial. Radiology. 2004;231:343-51. [PMID: 15031430]
- ^ "Imaging strategies for low-back pain: systematic review and meta-analysis : The Lancet". http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(09)60172-0/fulltext.
- ^ "BestBets: Early radiography in acute lower back pain". http://www.bestbets.org/bets/bet.php?id=867.
- ^ "www.acr.org". http://www.acr.org/SecondaryMainMenuCategories/quality_safety/app_criteria/pdf/ExpertPanelonNeurologicImaging/LowBackPainDoc7.aspx.
- ^ Choi BK, Verbeek JH, Tam WW, Jiang JY (2010). "Exercises for prevention of recurrences of low-back pain". Cochrane Database Syst Rev (1): CD006555. doi:10.1002/14651858.CD006555.pub2. PMID 20091596.
- ^ Delavier, Frédéric. Strength training anatomy. Human Kinetics Publishers, 2006. Print.}
- ^ http://www.spineuniverse.com/wellness/cigarette-smoking-its-impact-spinal-fusions
- ^ Mayo Clinic (2008). Back pain guide [on-line].
- ^ "Clinical Evidence: The international source of the best available evidence for effective health care". http://clinicalevidence.com/+ClinicalEvidence.com.(registration and log-in required)
- ^ French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ. Superficial heat or cold for low back pain. Cochrane Database Syst Rev. 2006:CD004750. [PMID: 16437495]
- ^ "Heat or Cold Packs for Neck and Back Strain: A Randomized Controlled Trial of Efficacy. Gregory Garra. 2010; Academic Emergency Medicine - Wiley InterScience". http://www3.interscience.wiley.com/journal/123372198/abstract.
- ^ a b http://orthoinfo.aaos.org/topic.cfm?topic=A00311
- ^ Atlas SJ. Nonpharmacological treatment for low back pain. Journal of Musculoskeletal Medicine. 2010;27(1):20-27.
- ^ Kovacs FM, Abraira V, Peña A, Martín-Rodríguez JG, Sánchez-Vera M, Ferrer E, et al. Effect of firmness of mattress on chronic non-specific low-back pain: randomised, double-blind, controlled, multicentre trial. Lancet. 2003;362:1599-604. [PMID: 14630439]
- ^ a b c d Koes B, van Tulder M (2006). "Low back pain (acute)". Clinical evidence (15): 1619–33. PMID 16973062. http://clinicalevidence.bmj.com/ceweb/conditions/msd/1102/1102.jsp.
- ^ a b c d e f van Tulder M, Koes B (2006). "Low back pain (chronic)". Clinical evidence (15): 1634–53. PMID 16973063. http://clinicalevidence.bmj.com/ceweb/conditions/msd/1116/1116.jsp.
- ^ "BestBets: Muscle relaxants for acute low back pain". http://www.bestbets.org/bets/bet.php?id=878.
- ^ Malanga GA, Dunn KR. Low back pain management: approaches to treatment. J Musculoskel Med. 2010;27:305-315.
- ^ Hagen KB, Hilde G, Jamtvedt G, Winnem M (2004). "Bed rest for acute low-back pain and sciatica". Cochrane Database Syst Rev (4): CD001254. doi:10.1002/14651858.CD001254.pub2. PMID 15495012.
- ^ Choi BK, Verbeek JH, Tam WW, Jiang JY (2010). "Exercises for prevention of recurrences of low-back pain". Cochrane Database Syst Rev (1): CD006555. doi:10.1002/14651858.CD006555.pub2. PMID 20091596.
- ^ a b Murphy AYMT, van Teijlingen ER, Gobbi MO (2006). "Inconsistent grading of evidence across countries: a review of low back pain guidelines". J Manipulative Physiol Ther 29 (7): 576–81, 581.e1–2. doi:10.1016/j.jmpt.2006.07.005. PMID 16949948. http://jmptonline.org/article/S0161-4754(06)00186-2/fulltext.
- ^ Assendelft WJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG (2004). "Spinal manipulative therapy for low back pain". Cochrane Database Syst Rev (1): CD000447. doi:10.1002/14651858.CD000447.pub2. PMID 14973958.
- ^ Chou R, Qaseem A, Snow V et al. (October 2, 2007). "Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society". Ann Intern Med 147 (7): 478–91. PMID 17909209. http://annals.org/cgi/content/full/147/7/478.
- ^ Bronfort G, Haas M, Evans R, Kawchuk G, Dagenais S (2008). "Evidence-informed management of chronic low back pain with spinal manipulation and mobilization". Spine J 8 (1): 213–25. doi:10.1016/j.spinee.2007.10.023. PMID 18164469.
- ^ Meeker W, Branson R, Bronfort G et al. (2007). "Chiropractic management of low back pain and low back related leg complaints" (PDF). Council on Chiropractic Guidelines and Practice Parameters. http://ccgpp.org/lowbackliterature.pdf. Retrieved 2008-03-13.
- ^ Assendelft WJJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG (2004). "Spinal manipulative therapy for low back pain". Cochrane Database Syst Rev (1): CD000447. doi:10.1002/14651858.CD000447.pub2. PMID 14973958.
- ^ Ernst E, Canter PH (2006). "A systematic review of systematic reviews of spinal manipulation". J R Soc Med 99 (4): 192–6. doi:10.1258/jrsm.99.4.192. PMID 16574972. PMC 1420782. http://www.jrsm.org/cgi/content/full/99/4/192. Lay summary – BBC News (2006-03-22).
- ^ Dagenais S, Mayer J, Wooley JR, Haldeman S (2008). "Evidence-informed management of chronic low back pain with medicine-assisted manipulation". Spine J 8 (1): 142–9. doi:10.1016/j.spinee.2007.09.010. PMID 18164462.
- ^ http://www.medicalnewstoday.com/articles/84989.php
- ^ Will This Patient Develop Persistent Disabling Low Back Pain? Roger Chou, MD; Paul Shekelle, MD, PhD JAMA. 2010;303(13):1295-1302. PMID: 20371789
- ^ Hayden JA, van Tulder MW, Malmivaara A, Koes BW (2005). "Exercise therapy for treatment of non-specific low back pain". Cochrane Database Syst Rev (3): CD000335. doi:10.1002/14651858.CD000335.pub2. PMID 16034851.
- ^ Weiss HR, Scoliosis-related pain in adults: Treatment influences. Eur J Phys Med Rehabil 1993; 3(3):91-94.
- ^ King SA (July 1, 2008). "Update on Treatment of Low Back Pain: Part 2". Psychiatric Times 25 (8). http://www.consultantlive.com/pain/article/10168/1167024.
- ^ Haake M, Müller HH, Schade-Brittinger C, et al. (2007). "German Acupuncture Trials (GERAC) for Chronic Low Back Pain: Randomized, Multicenter, Blinded, Parallel-Group Trial With 3 Groups". Arch. Intern. Med. 167 (17): 1892–8. doi:10.1001/archinte.167.17.1892. PMID 17893311.
- ^ Paul Little et al.,Randomised controlled trial of Alexander technique (AT) lessons, exercise, and massage (ATEAM) for chronic and recurrent back pain, British Medical Journal, August 19, 2008.
- ^ "BestBets: Are back schools effective in the management of chronic simple low back pain?". http://www.bestbets.org/bets/bet.php?id=1029.
- ^ Spinal Manipulative Therapy for Low Back Pain: A Meta-Analysis of Effectiveness Relative to Other Therapies * Willem J.J. Assendelft, * Sally C. Morton, * Emily I. Yu, * Marika J. Suttorp, * and Paul G. Shekelle Ann Intern Med June 3, 2003 138:871-881
- ^ Luciana AC Machado, Chris G Maher, Rob D Herbert, Helen Clare and James H McAuley. The effectiveness of the McKenzie method in addition to first-line care for acute low back pain: a randomized controlled trial. BMC Medicine, 8:10, doi:10.1186/1741-7015-8-10, 2010 here online
- ^ Audrey Long et al.: Specific Directional Exercises for Patients with Low Back Pain: A Case Series. Physiotherapy Canada 2008, Volume 60, Number 4 here online
- ^ Manca A, Dumville JC, Torgerson DJ, Klaber Moffett JA, Mooney MP, Jackson DA, Eaton S ; Randomized trial of two physiotherapy interventions for primary care back and neck pain patients: cost-effectiveness analysis. Rheumatology; 46:1495-15010, 2007 pdf
- ^ Schenk R, Jozefczyk, Kopf A ; A randomised trial comparing interventions in patients with lumbar posterior derangement. J Man & Manip Ther; 11:95-102, 2003
- ^ Machado LAC, de Souza MvS, Ferreira PH, Ferreira ML ; The McKenzie Method for low back pain. A systematic review of the literature with a meta-analysis approach Spine; 31:E254-E262, 2006
- ^ Long A, Donelson R, Fung T.: Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine 2004; 29, 2593-2602 here online
- ^ Clare HA, Adams R, Maher CG; A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother; 50(4):209-16, 2004
- ^ Petersen T, Kryger P, Ekdahl C, Olsen S, Jacobsen S.; The effect of McKenzie therapy as compared with that of intensive strengthening training for the treatment of patients with subacute or chronic low back pain: A randomized controlled trial. Spine; Aug 15;27(16):1702-9, 2002 here online
- ^ Cherkin DC, Deyo RA, Battie M, Street J, Barlow W.; A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med; Oct 8;339(15):1021-9, 1998 PDF
- ^ Chou R, Loeser JD, Owens DK, et al. (May 2009). "Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society". Spine 34 (10): 1066–77. doi:10.1097/BRS.0b013e3181a1390d. PMID 19363457.
- ^ Armon C, Argoff CE, Samuels J, Backonja M. Assessment: use of epidural steroid injections to treat radicular lumbosacral pain. Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2007; 68: 723–9.
- ^ a b http://www.ncbi.nlm.nih.gov/pubmed/11322842
- ^ "BestBets: Spinal fusion in chronic back pain". http://www.bestbets.org/bets/bet.php?id=909.
- ^ Mirza SK, Deyo RA. Systematic review of randomized trials comparing lumbar fusion surgery to nonoperative care for treatment of chronic back pain. Spine 2007; 32: 816–23.
- ^ "Overtreating chronic back pain: time to back off? Deyo.A et.al, Journal of the American Board of Family Medicine, March 2009". http://www.jabfm.org/cgi/content/full/22/1/62.
- ^ Furlan AD, Brosseau L, Imamura M, Irvin E (2002). "Massage for low back pain". Cochrane database of systematic reviews (Online) (2): CD001929. doi:10.1002/14651858.CD001929. PMID 12076429.
- ^ French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ (2006). "Superficial heat or cold for low back pain". Cochrane database of systematic reviews (Online) (1): CD004750. doi:10.1002/14651858.CD004750.pub2. PMID 16437495.
- ^ Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA (2005). "Comparing yoga, exercise, and a self-care book for chronic low back pain: a randomized, controlled trial". Ann. Intern. Med. 143 (12): 849–56. PMID 16365466.
- ^ Williams KA, Petronis J, Smith D, et al. (2005). "Effect of Iyengar yoga therapy for chronic low back pain". Pain 115 (1-2): 107–17. doi:10.1016/j.pain.2005.02.016. PMID 15836974.
- ^ Defrin R, Ben Benyamin S, Aldubi RD, Pick CG (2005). "Conservative correction of leg-length discrepancies of 10mm or less for the relief of chronic low back pain". Archives of physical medicine and rehabilitation 86 (11): 2075–80. doi:10.1016/j.apmr.2005.06.012. PMID 16271551.
- ^ Deshpande A, Furlan A, Mailis-Gagnon A, Atlas S, Turk D (2007). "Opioids for chronic low-back pain". Cochrane database of systematic reviews (Online) (3): CD004959. doi:10.1002/14651858.CD004959.pub3. PMID 17636781.
- ^ Urquhart DM, Hoving JL, Assendelft WW, Roland M, van Tulder MW (2008). "Antidepressants for non-specific low back pain". Cochrane Database Syst Rev (1): CD001703. doi:10.1002/14651858.CD001703.pub3. PMID 18253994.
- ^ Dubinsky RM, Miyasaki J (January 2010). "Assessment: efficacy of transcutaneous electric nerve stimulation in the treatment of pain in neurologic disorders (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology". Neurology 74 (2): 173–6. doi:10.1212/WNL.0b013e3181c918fc. PMID 20042705.
- ^ "BestBets: Prognosis in acute non-traumatic simple lower back pain". http://www.bestbets.org/bets/bet.php?id=860.
- ^ a b Urquhart DM, Hoving JL, Assendelft WW, Roland M, van Tulder MW (2008). "Antidepressants for non-specific low back pain". Cochrane Database Syst Rev (1): CD001703. doi:10.1002/14651858.CD001703.pub3. PMID 18253994.
- ^ about.com > Low Back Strain. Muscle strain of the lumbar spine By Jonathan Cluett, M.D. Updated January 10, 2010
- ^ ACSM's resources for clinical exercise physiology: musculoskeletal, neuromuscular, neoplastic, immunologic and hematologic conditions. (2009). Philadelphia, PA: Amer College of Sports.
- ^ Deyo RA, Mirza SK, Martin BI (November 2006). "Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002". Spine 31 (23): 2724–7. doi:10.1097/01.brs.0000244618.06877.cd. PMID 17077742.
- ^ Danforth Obstetrics and Gynecology Ninth Ed. Scott, James. Gibbs, et al, Ch. 1
- ^ Williams’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 8
- ^ Danforth Obstetrics and Gynecology Ninth Ed. Scott, James. Gibbs, et al, Ch. 1
- ^ http://www.americanpregnancy.org/pregnancyhealth/backpain.html
- ^ http://www.dynamicchiropractic.com/mpacms/dc/article.php?t=7&id=41386
Coccydynia
From Wikipedia, the free encyclopedia
| Coccydynia or Coccygodynia | |
|---|---|
| Classification and external resources | |
| ICD-10 | M53.3 |
| ICD-9 | 724.79 |
| eMedicine | pmr/242 |
Contents[hide] |
[edit] Synonyms
Coccydynia is also known as coccygodynia, coccygeal pain, coccyx pain, or coccaglia.[edit] Diagnosis
A number of different conditions can cause pain in the general area of the coccyx, but not all involve the coccyx and the muscles attached to it. The first task of diagnosis is to determine whether the pain is related to the coccyx. Physical examination, high resolution x-rays and MRI scans can rule out various causes unrelated to the coccyx, such as Tarlov cysts and pain referred from higher up the spine. Note that, contrary to most anatomical textbooks, most coccyxes consist of several segments: 'fractured coccyx' is often diagnosed when the coccyx is in fact normal or just dislocated at an intercoccygeal joint [1][2].A simple test to determine whether the coccyx is involved is injection of local anesthetic into the area. If the pain relates to the coccyx, this should produce immediate relief [3].
If the anesthetic test proves positive, then a dynamic (sit/stand) x-ray or MRI scan may show whether the coccyx dislocates when the patient sits [4].
Use of dynamic x-rays on 208 patients who gave positive results with the anesthetic test showed:
- 22% Posterior luxation (partial dislocation of the coccyx backwards when sitting)
- 5% Anterior luxation (partial dislocation of the coccyx forwards when sitting)
- 27% Hypermobility (excessive flexing of the coccyx forwards and upwards when sitting)
- 14% Spicule (bony spur) on the coccyx
- 31% Not possible to identify the cause of pain
[edit] Natural history
One way of classifying coccydynia is whether the onset was traumatic versus non-traumatic. In many cases the exact cause is not known (called idiopathic coccydynia).Coccydynia is often reported following a fall or after childbirth. In some cases, persistent pressure from activities like bicycling may cause the onset of coccyx pain.[5] Coccydynia due to these causes usually is not permanent, but it may become very persistent and chronic if not controlled.
Rarely, coccydynia is due to the undiagnosed presence of a sacrococcygeal teratoma or other tumor in the vicinity of the coccyx. In these cases, appropriate treatment usually involves surgery and/or chemotherapy.
[edit] Clinical features
Activities that put pressure on the affected area are bicycling, horseback riding, and other activities such as increased sitting that put direct stress on the coccyx. The medical condition is often characterized by pain that worsens with constipation and may be relieved with bowel movement. Rarely, even sexual intercourse can aggravate symptoms.[edit] Non-surgical treatment
Since sitting on the affected area may aggravate the condition, a cushion with a cutout at the back under the coccyx is recommended (the donut cushion traditionally recommended by doctors is generally useless for this condition). If there is tailbone pain with bowel movements, then stool softeners and increased fiber in the diet may help. For prolonged cases, anti-inflammatory or pain-relieving drugs may be prescribed. The use of anti-depressants such as Elavil (amiltriptyline) may help alleviate constant pain. Local nerve blocks are often beneficial. Tailbone pain doctors specializing in Physical Medicine and Rehabilitation at New Jersey Medical School have published that sometimes even just a single local nerve block injection at the ganglion impar can give 100% relief of coccydynia when performed under fluoroscopic guidance.[5][edit] Surgical treatment
In rare cases, surgery to remove the coccyx (coccygectomy) may be required. Typically, surgery is reserved for patients with cancer (malignancy) or those whose tailbone pain has failed to respond to nonsurgical treatment (such as medications by mouth, use of seat cushions, and medications given by local injections done under fluoroscopic guidance, as noted above). .[6][edit] See also
[edit] External links
- www.coccyx.org, website about coccydynia causes, treatments and coping with the condition
- Coccyx pain, tailbone pain, coccydynia at eMedicine
- Xray, MRI and other images about tailbone pain
[edit] References
- ^ Postacchini F, Massobrio M (October 1983). "Idiopathic coccygodynia. Analysis of fifty-one operative cases and a radiographic study of the normal coccyx". J Bone Joint Surg Am 65 (8): 1116–24. PMID 6226668.
- ^ Kim NH, Suk KS (June 1999). Clinical and radiological differences between traumatic and idiopathic coccygodynia.. 40. Yonsei Medical Journal. pp. 215–20. http://www.coccyx.org/medabs/kimsuk.htm.
- ^ Marx, Fred A. (1996). "Coccydynia/Levator Syndrome, A Therapeutic Test". Techniques in Coloproctology 4 (1). http://www.coccyx.org/medabs/marx.htm.
- ^ Maigne JY, Doursounian L, Chatellier G (December 2000). "Causes and mechanisms of common coccydynia: role of body mass index and coccygeal trauma". Spine 25 (23): 3072–9. doi:10.1097/00007632-200012010-00015. PMID 11145819. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0362-2436&volume=25&issue=23&spage=3072.
- ^ a b Foye P, Buttaci C, Stitik T, Yonclas P (2006). "Successful injection for coccyx pain". Am J Phys Med Rehabil 85 (9): 783–4. doi:10.1097/01.phm.0000233174.86070.63. PMID 16924191.
- ^ Foye PM (2007). "Reasons to delay or avoid coccygectomy for coccyx pain". Injury 38 (11): 1328. doi:10.1016/j.injury.2007.06.022. PMID 17884057.


Tidak ada komentar:
Posting Komentar